Scientists at the Helmholtz-Zentrum Dresden-Rossendorf (HZDR) and the National Center for Tumor Diseases Dresden (NCT/UCC), together with an international team of researchers, have succeeded in laboratory experiments to eradicate particularly radioresistant cancer cells of tumors in the head and neck area with the help of a targeted immunotherapy – the UniCAR T cell therapy. The researchers developed a new binding molecule that couples the UniCAR T cells to a specific surface feature of the cancer cells under investigation, thus activating them. In the future, combined radio-immunotherapy with UniCAR T cells might improve the chances of curing cancer patients with radioresistant tumors. The scientists published the results of their investigation in the journal Oncoimmunology (DOI 10.1080/2162402X.2020.1743036).
The National Center for Tumor Diseases Dresden (NCT/UCC) is a joint institution of the German Cancer Research Center (DKFZ), the University Hospital Carl Gustav Carus Dresden, Carl Gustav Carus Faculty of Medicine at TU Dresden and the Helmholtz-Zentrum Dresden-Rossendorf (HZDR).
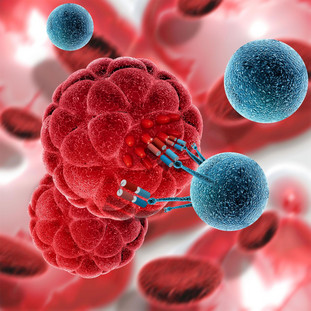
Radiation therapy, in addition to and in combination with surgery and chemotherapy, is one of the central pillars of cancer therapy and currently makes it possible to cure or control tumor diseases in many cases. However, highly resistant cancer stem cells within the tumor tissue present a particular difficulty. If it is not possible to completely destroy these cells, they can lead to renewed growth of the tumor after an initially successful therapy. In laboratory experiments, scientists have now succeeded in eradicating particularly radioresistant cancer cells in both test tube and mouse experiments using a targeted immunotherapy with UniCAR T cells. For their investigations, the researchers used cells from squamous cell carcinomas of the head and neck region - a cancer that originates from surface cells and to which the majority of malignant tumors in the head and neck region can be assigned.
"Our results show for the first time that in the future, immunotherapy using the UniCAR system, in combination with radiotherapy, could be specifically used to successfully combat particularly radioresistant tumor cells," says Prof. Michael Bachmann, Director at the HZDR Institute for Radiopharmaceutical Cancer Research, Professor of Translational Radiopharmacology at the TU Dresden and member of the extended board of directors of the NCT/UCC Dresden. "Patients with recurrent squamous cell carcinoma usually survive for less than six months. The poor prognosis is due to the resistance of certain cancer cells to radiation therapy. With the help of UniCAR T cell therapy, the chances of curing patients with radioresistant tumors could improve significantly in the future," said Prof. Mechthild Krause, Director of the Department of Radiation Oncology at the University Hospital Carl Gustav Carus Dresden and member of the Executive Board of the NCT/UCC Dresden.
The UniCAR technology is a further development of CAR T cell therapy, which is currently one of the most promising approaches in immunotherapy. In CAR T cell therapy, an artificial molecule called "CAR" ("chimeric antigen receptor") is incorporated into the T cells – white blood cells of the immune system – which acts as a navigation system to guide the cells to certain surface features of tumor cells. In the so-called UniCAR system, the altered T cell does not bind directly to the tumor cell. Rather, a special link (target module) is inserted between the immune and cancer cells, which enables the binding and hence the immune response. Since the artificially generated target modules are short-lived, the activity of the T cells can be controlled via the administered target module dose and the risk of serious side effects can be significantly reduced. In the present study, the scientists coupled the UniCAR T cells to the surface marker CD98, which is highly present on the radioresistant cancer cells under investigation, using a newly developed molecular linker. As an additional target for the immune cells, they used the cell membrane protein EGFR (epidermal growth factor receptor), for which a specific link was already present on the cancer cells.
The ability to control the activity of the altered immune cells is important, not least because the surface features of cancer cells that serve as targets for UniCAR T cells are often not exclusively present on tumors. For example, the target structure CD98, which is present on radioresistant squamous cell carcinoma cells of the head and neck area, is also present on the surface of the UniCAR T cells themselves – although to a much lesser extent. "We were able to show that the activity of the UniCAR system is initially directed against cells with a particularly high density of the respective target structure. Once the corresponding cells have been eliminated, the activity of the UniCAR T cells can be stopped by terminating the supply of the specific binding agent," explains Dr. Claudia Arndt, scientist at the HZDR.
The researchers initially plan to investigate the effectiveness of the UniCAR system on radiation resistant tumor cells in further laboratory experiments. If these experiments are successful, clinical trials might follow.
Publication:
Claudia Arndt, Liliana R. Loureiro, Anja Feldmann, Justyna Jureczek, Ralf Bergmann, Domokos Máthé, Nikolett Hegedüs, Nicole Berndt, Stefanie Koristka, Nicola Mitwasi, Frederick Fasslrinner, Chris Lamprecht, Alexandra Kegler, Anja Hoffmann, Tabea Bartsch, Ayşe Sedef Köseer, Gary Egan, Marc Schmitz, Vaclav Hořejší, Mechthild Krause, Anna Dubrovska, Michael Bachmann: UniCAR T cell immunotherapy enables efficient elimination of radioresistant cancer cells,
OncoImmunology, DOI: https://doi.org/10.1080/2162402X.2020.1743036
Press Contact:
Dr. Anna Kraft
Nationales Centrum für Tumorerkrankungen Dresden (NCT/UCC)
Presse- und Öffentlichkeitsarbeit
Tel.: +49 (0)351 458-5548
E-Mail: anna.kraft@nct-dresden.de
www.nct-dresden.de